Diabetes care in SA not up to scratch
Over 4 million South Africans suffer from diabetes, and few are receiving the care they need. According to Dr Patrick Ngassa Piotie, chairperson of the Diabetes Alliance and co-founder of Tuks’ Diabetes Research Centre, improving diabetes care in South Africa requires several factors to be in place, including patient education, training for healthcare workers, the use of modern drugs and technologies, and the deployment of diabetes nurse educators.

Medical Academic (MA): So, I suppose the first question would be, in general terms, what is your perspective on the current state of diabetes treatment in South Africa?
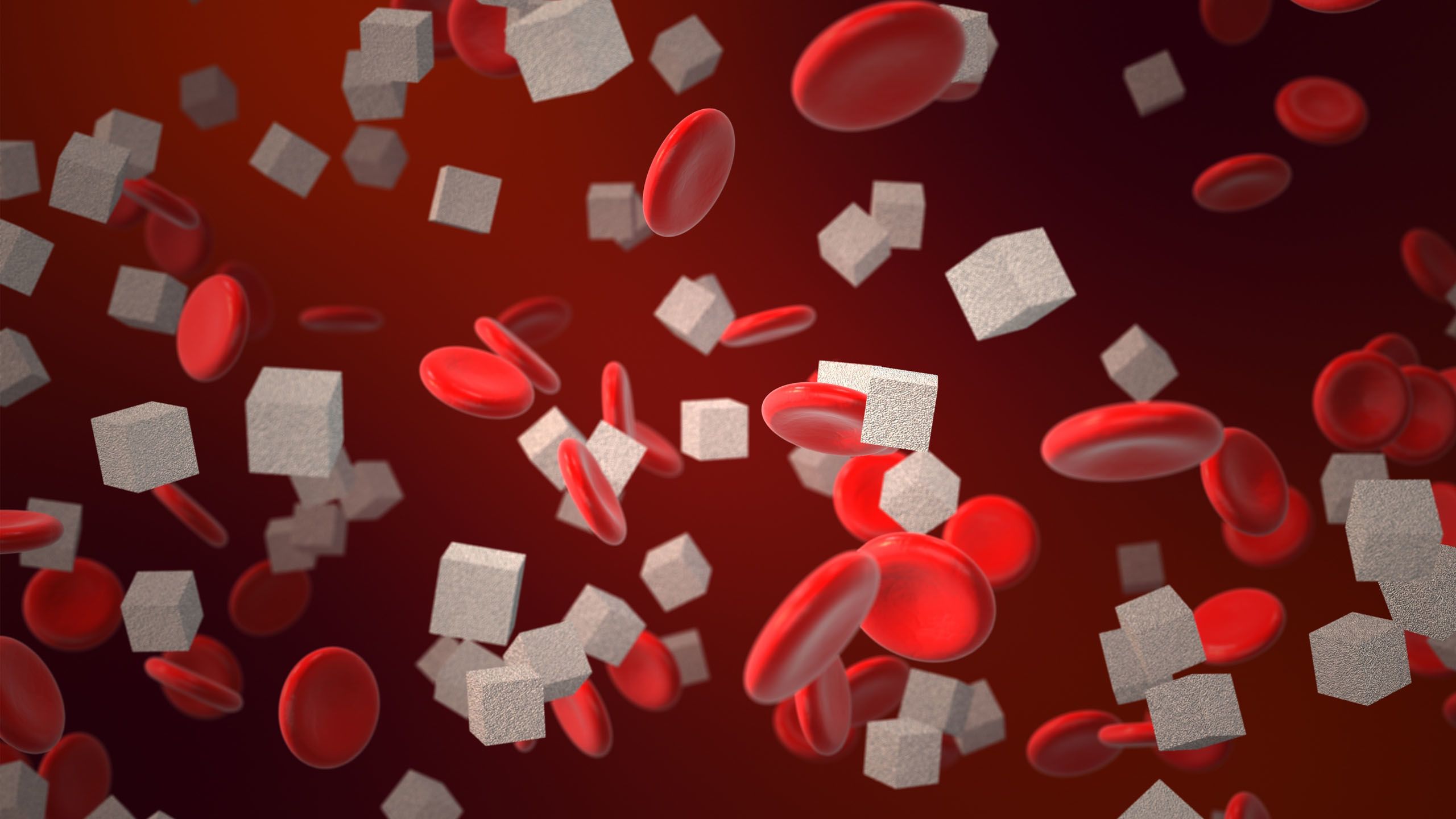
Dr Patrick Ngassa Piotie (PNP): To provide some background, diabetes has become a major public health crisis in South Africa. The most recent statistics from StatsSA show that diabetes is now leading in terms of the number of deaths in South Africa, and it's likely this will continue in the foreseeable future. So diabetes deserves our full attention. .
When we look at the quality of diabetes care here, the limited studies available, often sporadic or regional research rather than systematic, reveal a troubling situation. These localised studies, whether from districts in Gauteng, parts of the Western Cape, or KwaZulu-Natal, all point to significant gaps. Diabetes management is simply not where it should be, especially in terms of blood glucose control.
The rate of glucose control, measured through HbA1c, hovers between 13 and 30 percent. This means around 70 percent of people with diabetes are exposed to persistently high glucose levels, even though diabetes management shouldn’t be overly complex. Diabetes has been around for many years, and we have a range of drugs available in the public sector to manage it.
If we also consider other treatment targets for people with diabetes, like hypertension and lipid levels, the picture becomes even more concerning. For someone with diabetes, care isn’t only about managing blood glucose; hypertension and cholesterol often need control as well. But even these targets aren’t being met in the public sector. And surprisingly, when we compare public and private sectors, studies indicate that diabetes care outcomes in the private sector aren’t much better. Despite private healthcare being better resourced, patients in private care also receive suboptimal diabetes management.
MA: So, regardless of whether a South African is receiving diabetes care in the public or private sector, you’re saying that the outcomes are generally not where they need to be?
PNP: Exactly. Patients are still exposed to high levels of preventable complications, which is a serious challenge.

"Consistent, high-quality education could go a long way, but it’s currently lacking."

MA: What steps do you think we could take to improve the quality of care in both the public and private sectors?
PNP: Improving diabetes care has been a focus for groups like the Society for Endocrinology, Metabolism and Diabetes of South Africa (SEMDSA), the Department of Health, and other advocates, especially with initiatives like the Diabetes Alliance. We launched the Diabetes Summit in 2021, bringing together stakeholders to discuss solutions.
One initiative the Department of Health has introduced is the National Strategic Plan for the Prevention and Control of Non-Communicable Diseases, which includes diabetes and hypertension. For the first time, this plan sets clear diabetes targets, called the "1960-50" framework.
The goals are that 90 percent of people living with diabetes should know their status, at least 60 percent should be connected to care or receiving interventions, and 50 percent should be adequately controlled. Presently, our control rates sit between 30 and 50 percent, so the aim is to improve this. As the Diabetes Alliance, we view this as a positive step; it gives us a starting point, even if there’s still a long way to go.
At the 2023 Diabetes Summit, we looked specifically at how to achieve these targets. Prevention is a major component—strengthening measures like the sugar tax and investing more in prevention efforts. For those already living with diabetes, we need to improve education. Currently, diabetes education in the public sector, and to some extent in the private sector, is inconsistent. It depends on whether the healthcare provider is well-trained, passionate, and whether the patient is in a rural or urban area.
MA: So, increasing education for people with diabetes could be one way forward?
PNP: Absolutely. International guidelines for diabetes care emphasise person-centred care, because most people with diabetes spend only a small amount of time in healthcare facilities. Most of their time, they’re managing their diabetes independently. Therefore, it’s crucial to empower people with diabetes to manage their condition when they’re not with healthcare workers.
Consistent, high-quality education could go a long way, but it’s currently lacking. In some private sector facilities, they have diabetes nurse educators, but this role isn’t widespread, and in the public sector, it isn’t even recognised by the Department of Health or relevant unions. We believe introducing diabetes nurse educators could ensure that people with diabetes receive the guidance they need. We can’t expect doctors and nurses, who are already stretched thin, to take on this additional role.
In terms of treatment itself, SEMDSA has put out guidelines, but studies show these are not widely implemented, often because healthcare workers haven’t received the appropriate training. Capacity building and training in comprehensive diabetes management—whether at primary, secondary, or tertiary care levels in both the public and private sectors—should be strengthened.
MA: In the public sector, do you think the available drugs are adequate?
PNP: Unfortunately, many of the drugs used in the public sector are quite outdated. They are still somewhat effective, but if we think of it in terms of technology—just because landline phones still work doesn’t mean we shouldn’t adopt mobile phones. Similarly, there are newer diabetes drugs that offer significant benefits, including renal and cardiovascular protection, and better target achievement. One of our requests to the Department of Health has been to introduce these newer drugs into the public sector.
Then there’s diabetes technology, such as continuous glucose monitoring, which can be a game-changer, especially for people on insulin who may need to check their glucose levels multiple times a day. Continuous glucose monitoring allows people to gain insights into their condition and manage it more effectively, avoiding frequent finger pricking. These technologies could make diabetes management more comfortable and effective.