Original study
Outcomes of uveitic cataract surgery in a cohort of South African children
C Kennedy MBBCh, Mmed (UCT), FC Ophth (SA), Dip Ophth (SA), Registrar, division of Ophthalmology, University of Cape Town, South Africa.
ORCID: http://orcid.org/ 0009-0009-4777-4322
J Steffen MBChB, FCOphth (SA), MMed (Ophth); Consultant Ophthalmologist, Vitreoretinal Surgery and Uveitis, Groote Schuur Hospital, University of Cape Town, South Africa.
ORCID: http://orcid.org/ 0000-0003-0364-3338
C Tinley MBChB, FRCOphth (London); Paediatric Ophthalmologist, Associate Professor, Division of Ophthalmology, University of Cape Town, South Africa.
ORCID: http://orcid.org/ 0000-0001-5817-7122
Corresponding author: Dr Clare Kennedy; email: clarekenned@gmail.com

Introduction
Cataract formation is the most common ocular complication observed in paediatric patients with uveitis and can result in significant visual impairment.¹ Uveitis in children has a relatively severe course and is more likely to lead to vision loss.² Amblyopia, extended burden of disease over time, delayed diagnosis and difficult examinations are challenges unique to uveitis in childhood.³,⁴ In a large multicentre, multi-ethnic study in the United States by Smith et al., the baseline prevalence of legal blindness in children due to uveitis was 9.23% and visual impairment (6/30 VA or less) was 13.3%.⁵
Cataracts form in response to chronic inflammation, or as a side-effect of prolonged use of steroid medication. The surgical management of cataracts in paediatric patients with uveitis poses many challenges. There are differing opinions with regards to the surgical approach, namely lensectomy with PPV, or anterior approach lensectomy with anterior vitrectomy.¹ Whether to insert an IOL or leave the patient aphakic also remains controversial.¹ In the early 1990’s, the use of an IOL in paediatric uveitic eyes was associated with significant inflammation, development of intractable glaucoma, cyclitic membrane formation, hypotony, and phthisis.⁶,⁷ In these eyes, the degree of fibrosis around the IOL led to cocooning of the IOL inside the capsular bag.⁸,⁹ More recent studies have revealed good postoperative outcomes in children with PCIOL implantation.¹⁰ On the contrary, others have concluded that PPV and lensectomy, without intraocular lens insertion, is the preferred surgical option, especially in cases where cyclitic membranes or vitritis are present.¹¹ They note that visual acuity and post-operative control of inflammation was significantly improved with PPV. Proposed reasons for this include removal of a diseased vitreous body and a reduced degree of macular oedema.¹²
It is important to determine the long-term outcomes (especially visual outcomes and the need for ongoing immunosuppression treatment) in paediatric uveitic patients undergoing cataract surgery and compare outcomes of different surgical management approaches. The post-operative complication profile should also be researched and compared. Possible postoperative complications include glaucoma, CMO, epiretinal membrane formation, posterior capsular opacification (PCO), retinal detachment, hypotony, choroidal neovascular membrane formation and vitreous haemorrhage.¹ There is no published data with regards to the outcomes of uveitic cataract surgery in South African children. This study was done to report on current management practices and visual outcomes in a cohort of South African children and compare these to international studies.
Methods
A retrospective patient folder review, from 01 January 2010 to 31 December 2020, was conducted of paediatric patients, managed at the Red Cross War Memorial Children’s Hospital (RCWMCH), a tertiary referral hospital in Cape Town, South Africa. Institutional ethical review board approval at Groote Schuur Hospital (GSH) was obtained (HREC REF 405/2020). Inclusion criteria were children up to the age of 13 years who had cataract surgery for uveitic cataracts. Exclusion criteria included: children older the age of 13 years at time of surgery, post operative follow up time of less than one year, Fuchs’ uveitis syndrome and post traumatic uveitis. Data parameters collected included: patient age at diagnosis and gender. Anatomical classification, aetiology, activity of uveitis was noted as well as complications of uveitis present at first review. BCVA at presentation and final postoperative visit was noted, as well as surgical details, including surgical approach, IOL insertion, intra- and postoperative complications.
The objective of the study was to determine the peri- and postoperative outcomes of paediatric uveitic cataract surgery. The primary aim was to determine the postoperative BCVA and change from baseline. Secondary aims included review of the intraoperative and postoperative complications, postoperative immunosuppression requirements and side-effects, and need for secondary surgical procedures. Due to the retrospective nature of the study and small patient group, descriptive statistical methods were used in data analysis.
In terms of visual function, pre and post operative BCVA was recorded.
Age-appropriate testing was done, and VA values converted to Snellen acuity. If the child was too young for charts, it was noted if central, steady fixation was maintained, if they could follow objects, or if they could identify 100’s and 1000’s. Immunosuppressive treatment regimens pre and post operatively were documented. The complication profile of this disease entity and the medical and surgical management was assessed. Complications of uveitis at first presentation included: cataracts, band keratopathy, glaucoma, macular oedema, posterior synechiae and retinal detachment. Complications of medical immunosuppression therapy included: Cushing syndrome, diabetes mellitus, raised intraocular pressure (IOP) and glaucoma and opportunistic infections. Intra and post operative complications of cataract surgery were noted including retinal breaks, retinal detachment, PCO, CMO, hypotony, ocular hypertension and glaucoma and worsened inflammation requiring more aggressive immunosuppressant therapy.
Patients managed at RCWMCH were done so by a consultant ophthalmologist and paediatric rheumatologist. Patients selected for PPV approach were reviewed by and operated on by a vitreo-retinal specialist at GSH. Two patients had their surgery in private by a consultant vitreoretinal surgeon, and one patient had their initial surgery at a secondary level hospital. Patients had a comprehensive ocular examination, and the uveitis was graded and recorded according to the standard uveitis nomenclature (SUN) criteria. All patients with a poor fundus view with a slit lamp or indirect ophthalmoscope had a B scan ultrasound to assess for possible vitritis, retinal membranes or detachment.
Preoperatively, patients seen at RCWMCH and GSH were only booked for surgery after control of inflammation had been achieved (for at least three months) unless the risk of amblyopia, or bilateral visual impairment necessitated early surgery. A standard perioperative steroid treatment protocol was followed. Preoperatively, all patients received 1mg/kg oral prednisone for a week, and this was continued and tapered over a month post operatively.
The surgical technique for the anterior approach cataract extraction cases was as follows: clear corneal incisions, circumlinear capsulorhexis, lens aspiration. If the decision was made to insert an IOL, a PCIOL Acrysoft IOL (Alcon Laboratories, Fort Worth, TX) placed in the capsular bag. A primary posterior capsulotomy with a limited anterior vitrectomy was performed in all cases done at RCWHCH. Intracameral antibiotics and subtenons depot steroid were given and all wounds were sutured. The technique for PPV lensectomies included a 23G or 25G vitrectomy and lens washout with the vitreous cutter through an anterior or posterior approach. Synechiolysis and iris retractors were used as needed. This was followed with a total or subtotal capsulectomy and posterior vitrectomy. All patients were left aphakic. Wounds were sutured, and all patients received intravitreal antibiotics and dexamethasone at the end of the procedure.
Amblyopia therapy was initiated where indicated. Aphakic refractive correction was given in the form of contact lenses or spectacles.
Results
Patient characteristics
A total of 18 eyes from 14 patients were enrolled in the study. Eight (57.1%) of the patients were male and eight patients (57.1%) had bilateral involvement of uveitis. The mean age at uveitis diagnosis was five years, five months (range one year, nine months to 10 years) and the mean age at cataract surgery was six years, five months (range two years, six months to 10 years, nine months).
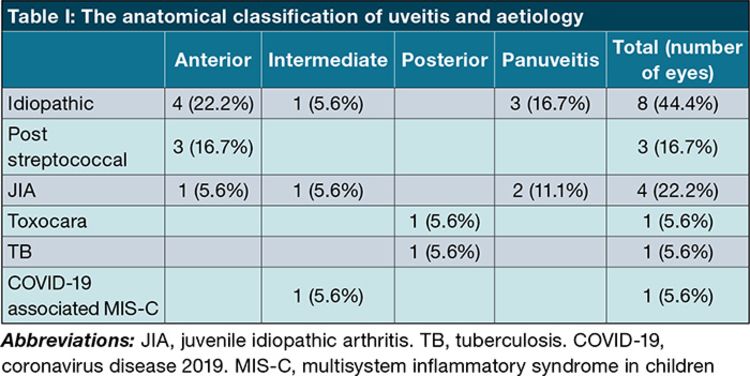
The anatomical classification of uveitis and aetiology are shown in Table I.
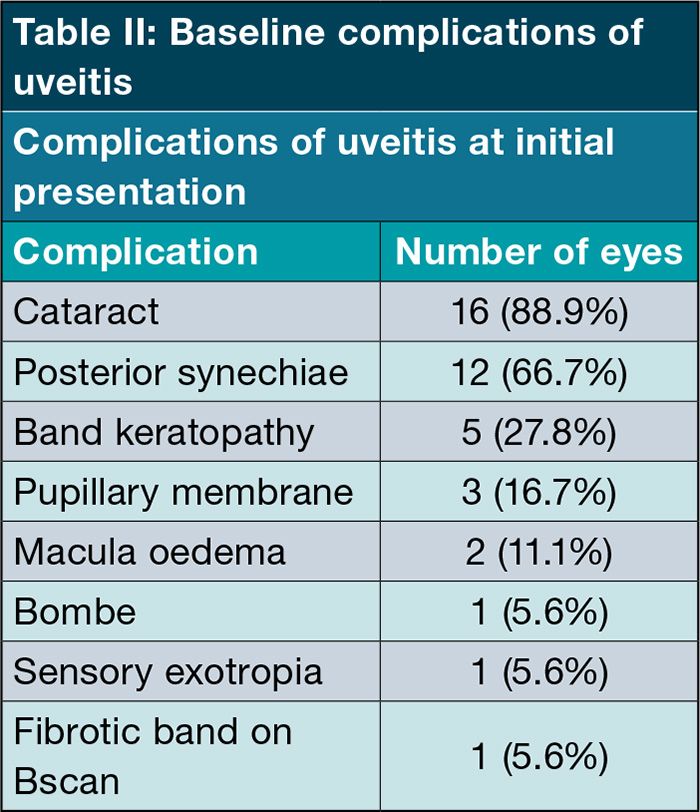
The complications of uveitis at initial presentation were mainly cataracts and posterior synechiae and are represented in Table II.
Uveitis treatment prior to cataract surgery
Prior to surgery, three patients were on topical steroid treatment only, two patients were receiving topical and oral steroid treatment and one patient was on no treatment. Nine patients were receiving additional systemic immunosuppression (seven patients receiving methotrexate and two patients receiving methotrexate and biological agents) as well as oral and topical steroids. Twelve patients (15 eyes) had good control of uveitis inflammation for at least three months prior to cataract surgery, whilst two patients (three eyes) had surgery whilst the uveitis was not completely controlled (one patient required early surgery bilaterally as signs of amblyopia were present at the first review, and in one patient, who received cataract surgery at a district hospital, it is unclear whether preoperative control of inflammation was adequate.)
Cataract surgery: Three eyes (16.7%) had anterior approach cataract surgeries with IOL insertion, and 15 eyes (83.3%) had PPV lensectomies and were left aphakic. Two patients had bilateral cataract surgery and two patients with bilateral cataracts had undergone surgery in one eye, were awaiting surgery in the second eye at the time of data collection. Two of the anterior segment surgeries were performed by a specialist paediatric ophthalmologist, and one by a general ophthalmologist. All PPVs were performed by a vitreoretinal surgeon.
Visual outcomes
Figure 1 is a representation of the improvement of preoperative to postoperative BCVA. All eyes showed an improvement in BCVA postoperatively. Of the 18 eyes operated, two patients (each had one eye operated) were unable to be tested using a chart as they were preverbal. The first patient’s vision in that eye was measured as central steady and maintained and the other patient’s vision was recorded as fixing and following and able to do 100s and 1000s. Out of the 16 eyes operated where BCVA could be quantified, 11 eyes (68.8%) achieved BCVA equal or better than 6/12 with 10 eyes (62.5%) achieved a vision of 6/9 or 6/6. The mean gain in BCVA was 5 Snellen lines (range 2-7 lines). Four eyes had a postoperative BCVA of 6/60 or worse. Reasons for poorer visual outcomes included: pre-existing amblyopia, retinal detachment, CMO and glaucoma. Poor treatment compliance missed appointments and difficult social circumstances were compounding factors.
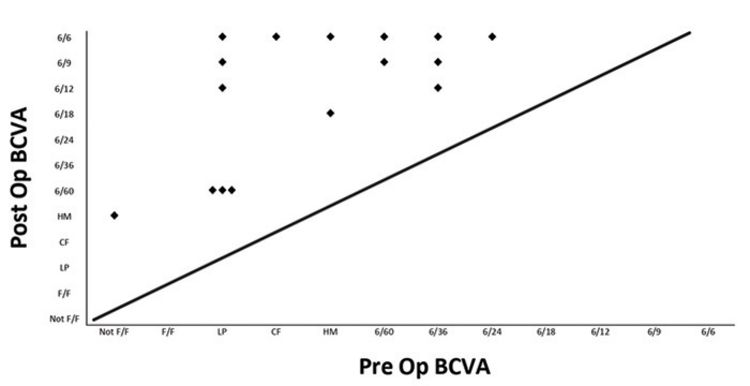
Figure 1: Improvement of preoperative to postoperative BCVA
Figure 1: Improvement of preoperative to postoperative BCVA
Complications
The only intraoperative complication included an iatrogenic retinal break during one PPV lensectomy. Cryotherapy was done intra operatively and silicone oil was inserted. This patient later had removal of silicone oil with insertion of a 360-degree encircling band and achieved a final BCVA of 6/12.
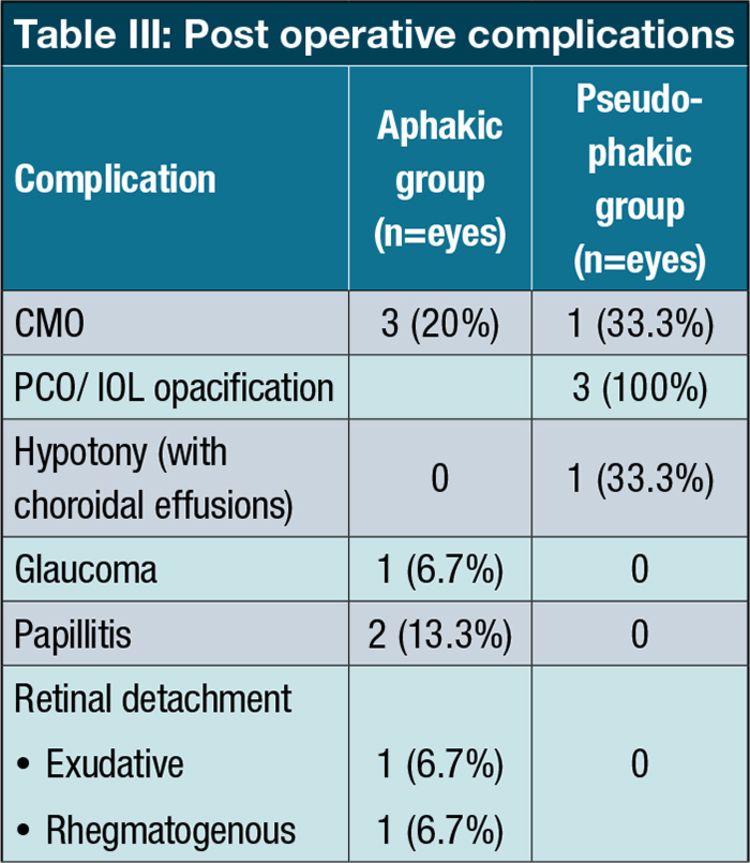
Post operative complications are shown in Table III
Post operatively, five eyes were noted to have worsened inflammation, [three eyes (20%) were in the aphakic group and two (66.7%) in the pseudophakic group. Post operatively, five patients were using biologics as part of their treatment regimen. In one of the eyes with disc oedema, this became chronic with macular star formation and prepapillary gliosis (this patient had poor social circumstances and a history of defaulting treatment). A second patient who defaulted treatment and follow up visits, developed an exudative retinal detachment. One eye developed a rhegmatogenous retinal detachment eight years post PPV lensectomy surgery and underwent PPV with retinal detachment repair. A successful outcome was achieved with a final BCVA of 6/9. Four eyes (22.2%) had ocular hypertension (thought to be a steroid response).
In terms of systemic complications of steroid treatment, five patients (35.7%) developed Cushing disease and one patient developed insulin dependent diabetes mellitus. One patient on steroid and steroid sparing immunosuppression contracted multi drug resistant tuberculosis.
Of the three eyes that had anterior approach cataract surgeries with IOL insertions, two needed IOL removal and PPV. The first eye had anterior and posterior fibrotic membrane formation encapsulating the IOL and worsening inflammation post operatively. After the second surgery, this patient developed CMO. The indication for the second eye needing IOL removal was severe PCO as well as CMO, hypotony with choroidal effusions and persistent post operative inflammation. This patient had ongoing inflammation post PPV and IOL removal as well. The patient who retained their IOL had worsening inflammation post operatively and visually significant IOL deposits requiring long term topical steroid dependence. This patient was considered for a PPV with IOL removal, but the IOL deposits cleared on topical prednisolone 1% twice daily. With regards to secondary surgical procedures required, two eyes underwent PPV with removal of the IOL. One eye had removal of silicone oil and insertion of 360-degree encircling band and one eye had a goniotomy.
Discussion
Published literature has shown that a variety of clinical and management factors affect the final visual outcome of paediatric uveitic cataract surgery.¹⁹ The timing, surgical approach, insertion or not of an IOL and long-term control of inflammation are key to good outcomes.¹ There is consensus in the literature that good pre operative control of uveitis (absent of activity for at least three months pre op) is vital for long term success.1,13,14,15 In some cases severe visual impairment and amblyopia risk necessitate earlier surgery. The most common category of uveitic cataract in our study was idiopathic, even though the most common cause of uveitis at our tertiary referral centre is juvenile idiopathic arthritis associated uveitis (JIAU).¹⁷ Almost half (44.4%) of our study patients had anterior uveitis. Four studies (AlAmeer, Smith, Edelsten, Rosenberg) noted the same finding.⁵,⁹,²⁰,²¹
Smith et al. showed the most common complications of uveitis at initial presentation were posterior synechiae (33.8%), band keratopathy (27.8%) and cataracts (19.9%).⁵ In our study, cataract formation (88.9%) was the most common baseline complication of uveitis, followed by posterior synechiae (66.7%) and band keratopathy (27.2%).
In our study, the most frequent postoperative complication was CMO (22.2%). In a recent study by Al Ameer et al., glaucoma was noted as the most common complication.¹⁹ Yangzes et al. showed that PCO was the most common post operative complication.¹
Gautam et al. showed reduced macular oedema post PPV.¹⁶ This is in contrast to the study by Yangez et al. which showed that CMO was significantly less in the pseudophakic group, which could be attributed to the fact that the anterior hyaloid face was not breached in majority of these patients.¹ Of the four eyes that developed CMO post operatively in our study, three had undergone PPVs and been left aphakic and one had undergone anterior surgery with IOL insertion.
There is evidence suggesting that IOL insertion is a favourable option. Terrada et al. recommended intraocular lens insertion to negate the risk of aniseikonia and amblyopia associated with unilateral aphakia.¹⁴ Lam et al. commented that: “with adequate long-term preoperative and postoperative control of intraocular inflammation with systemic immunosuppressive therapy in addition to intensive topical corticosteroid treatment, children with JIA-associated uveitis can demonstrate favourable surgical outcomes after cataract surgery with posterior chamber IOL”.¹³ Topical corticosteroid treatment was given hourly or two hourly for a median duration of 8.5 weeks post operatively.¹³ Another study by Terrada et al., concluded that: “uveitis is not a formal contraindication to primary IOL implantation in the management of paediatric cataract surgery in cases with full control of intraocular inflammation”.¹⁴ Sijssens et al. (a study looking at cataract surgery outcomes in a group of children with JIA associated uveitis) concluded that there was no difference in development of ocular complications in PCIOL insertion compared to aphakia.²³
In a recent study however by AlAmeer et al., which reviewed data from 26 patients (39 eyes), primary IOL implantation was shown to be a statistically significant risk factor for unsuccessful outcome.¹⁹ Our study showed the patients left aphakic had a better long-term outcome with less complications and less need for secondary surgical procedures. It is important to note however that the pseudophakic group was too small for statistical analysis.
The long-term post operative BCVA results in our study were excellent, with all patients showing improvement with a mean gain in VA of 5 lines. The VA of 68.8% of eyes was 6/12 or better, 62.5% achieved a VA of 6/9 or 6/6. These results are similar to other recent studies.¹,¹⁹ Yangzes et al. showed that 55% of patients achieved a BCVA of 6/12 or better.¹ AlAmeer et al. showed that 64% of the patients achieved BCVA equal to or better than 6/18.¹⁹ Limitations of our study were the small study size and its retrospective nature. There were also a limited number of patients who had an IOL inserted, so it was difficult to draw accurate comparisons to the aphakic group.
Conclusion
Post operative visual improvement was noted in all our study patients, with 68.8% of eyes achieving a BCVA equal or better than 6/12. This concurs with the current literature. The three patients who had IOL’s inserted had severe post-operative complications, two of which required explanation. There is evidence in the literature however to suggest that IOL insertion can give favourable results. Further prospective studies are warranted with larger patient numbers to further research and improve surgical techniques and management strategies for paediatric uveitic cataracts.
References
- Yangzes S, Seth NG, Singh R, Gupta PC, Jinagal J, Pandav SS, Gupta V, Gupta A, Ram J. Long-term outcomes of cataract surgery in children with uveitis. Indian J Ophthalmol 2019;67:490.
- Cunningham ET., Jr Uveitis in children. Ocul Immunol Inflamm. 2000;8:251–61.
- Smith JR. Management of uveitis in pediatric patients: special considerations. Paediatr Drugs. 2002;4:183–9.
- Holland GN, Stiehm ER. Special considerations in the evaluation and management of uveitis in children. Am J Ophthalmol. 2003;135:867–78.
- Smith JA, Mackensen F, Sen HN, Leigh JF, Watkins AS, Pyatetsky D, Tessler HH, Nussenblatt RB, Rosenbaum JT, Reed GF, Vitale S, Smith JR, Goldstein DA. Epidemiology and course of disease in childhood uveitis. Ophthalmology. 2009 116(8):1544-51.
- Angeles-Han S, Yeh S. Prevention and management of cataracts in children with juvenile idiopathic arthritis-associated uveitis. Curr Rheumatol Rep. 2012;14:142-9.
- Foster CS, Barrett F. Cataract development and cataract surgery in patients with juvenile rheumatoid arthritis-associated iridocyclitis. Ophthalmology.1993;100:809-17.
- Cassidy J, Kivlin J, Lindsley C, Nocton J. Ophthalmologic examinations in children with juvenile rheumatoid arthritis. Pediatrics. 2006;117:1843-5.
- Probst LE, Holland EJ. Intraocular lens implantation in patients with juvenile rheumatoid arthritis. Am J Ophthalmol. 1996;122:161-70.
- Lundvall A, Zetterstrom C. Cataract extraction and intraocular lens implantation in children with uveitis. Br J Ophthalmol 2000;84:791-3.
- BenEzra D, Cohen E. Cataract surgery in children with chronic uveitis. Ophthalmology 2000;107:1255-60.
- Giuliari, G., Chang, P., Thakuria, P. Pars plana vitrectomy in the management of paediatric uveitis: the Massachusetts eye research and surgery Institution experience. Eye 2010;24:7-13.
- Lam LA, Lowder CY, Baerveldt G, Smith SD, Traboulsi EI. Surgical management of cataracts in children with juvenile rheumatoid arthritis-associated uveitis. Am J Ophthalmol. 2003;135(6):772-8.
- Terrada C, Julian K, Cassoux N, Prieur AM, Debre M, Quartier P, LeHoang P, Bodaghi B. Cataract surgery with primary intraocular lens implantation in children with uveitis: long-term outcomes. J Cataract Refract Surg. 2011;37(11):1977-83.
- Ram J, Kaushik S, Brar GS, Gupta A, Gupta A. Phacoemulsification in patients with Fuchs’ heterochromic uveitis. J Cataract Refract Surg. 2002;28(8):1372-8.
- Gautam N, Singh R, Agarwal A, Yangzes S, Dogra M, Sharma A, Bansal R, Gupta V, Dogra MR, Gupta A. Pattern of Pediatric Uveitis at a Tertiary Referral Institute in North India. Ocul Immunol Inflamm. 2018;26(3):379-385.
- Slamang, W., Tinley, C., Brice, N. et al. Paediatric non-infectious uveitis in Cape Town, South Africa: a retrospective review of disease characteristics and outcomes on immunomodulating treatment. Pediatr Rheumatol 2021;19:50.
- The Infant Aphakia Treatment Study Group. Comparison of contact lens and intraocular lens correction of monocular aphakia during infancy. A randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 years. JAMA Ophthalmol. 2014;132:676–82.
- AlAmeer AM, Al Shamrani M. Outcome of cataract surgery in pediatric uveitis (experience at King Khalid Eye Specialist Hospital). Oman J Ophthalmol. 2022;15(1):43-48.
- Edelsten C, Reddy MA, Stanford MR, Graham EM. Visual loss associated with pediatric uveitis in English primary and referral centers. Am J Ophthalmol. 2003;135:676-80.
- Rosenberg KD, Feuer WJ, Davis JL. Ocular complications of pediatric uveitis. Ophthalmology. 2004;111:2299-306.
- Quiñones K, Cervantes-Castañeda RA, Hynes AY, Daoud YJ, Foster CS. Outcomes of cataract surgery in children with chronic uveitis. J Cataract Refract Surg. 2009;35:725-31.
- Sijssens KM, Los LI, Rothova A, Schellekens PA, van de Does P, Stilma JS, de Boer HJ. Long-term ocular complications in aphakic versus pseudophakic eyes of children with juvenile idiopathic arthritis-associated uveitis. Br J Ophthalmol 2010;94:1145-9
- Phatak S, Lowder C, Pavesio C. Controversies in intraocular lens implantation in pediatric uveitis. J Ophthal Inflamm Infect 2016;6:12.
- Gangaputra S, Newcomb C, Armour R, Choi D, et al. Long-term visual acuity outcomes following cataract surgery in eyes with ocular inflammatory disease. Br J Ophthalmol. 2023;2022-322236:10.1136.
- Guindolet D, Dureau P, Terrada C, Edelson C, Barjol A, Caputo G, LeHoang P, Bodaghi B. Cataract Surgery with Primary Lens Implantation in Children with Chronic Uveitis. Ocul Immunol Inflamm. 2018;26(2):298-304.
