Reducing stroke risk for AFib patients
The risk of stroke is greatly elevated among patients with atrial fibrillation.

Atrial fibrillation (AFib) poses a significant challenge in stroke prevention due to its impact on blood flow dynamics. In sinus rhythm, the heart efficiently pumps blood with each atrial contraction, minimising the risk of clot formation. However, AFib disrupts this rhythm, causing reduced blood flow velocities in the atria, leading to blood pooling and an increased risk of clot formation.
These clots, especially from the left atrial appendage (LAA), can dislodge and cause serious complications, including stroke. Indeed, over 90% of thrombi in AFib patients originate from the LAA, underscoring its critical role in stroke risk assessment.
AFib is a major cause of cardioembolism, accounting for 35% of non-lacunar strokes and 15-24% of all ischemic strokes. AFib-related strokes are nearly twice as likely to be fatal, generally more severe, and more likely to recur compared to non-AF strokes.
To assess stroke risk in AF patients, the CHA2DS2-VASc score is commonly used. This scoring system evaluates factors such as age, congestive heart failure, hypertension, diabetes, prior stroke, and other comorbidities. Higher scores indicate a greater risk of stroke, with anticoagulation therapy recommended for men with scores of 2 or higher and for women with scores of 3 or higher.
Beyond the CHA2DS2-VASc score, there is growing interest in the anatomical characteristics of the LAA. Preliminary data suggest that LAA size and shape may influence stroke risk. Smaller LAAs typically present a lower risk due to reduced blood stasis, while more complex or trabeculated LAAs may have a higher risk of clot formation. Despite these findings, LAA anatomy is not yet a standard clinical measure due to limited large-scale validation.


STROKE RISK IN AFIB
Managing stroke risk in AF involves various strategies. Anticoagulation therapy remains central, with direct oral anticoagulants (DOACs) such as dabigatran, rivaroxaban, apixaban, and edoxaban preferred over warfarin for most patients. DOACs offer predictable dosing and fewer dietary restrictions, although warfarin is still used for patients with mechanical heart valves or significant mitral stenosis.
While DOACs simplify management compared to warfarin, they require careful monitoring, especially in patients with renal impairment. Anticoagulants increase bleeding risks, and poor adherence to therapy can lead to suboptimal protection against stroke, with potentially devastating consequences if a stroke occurs.
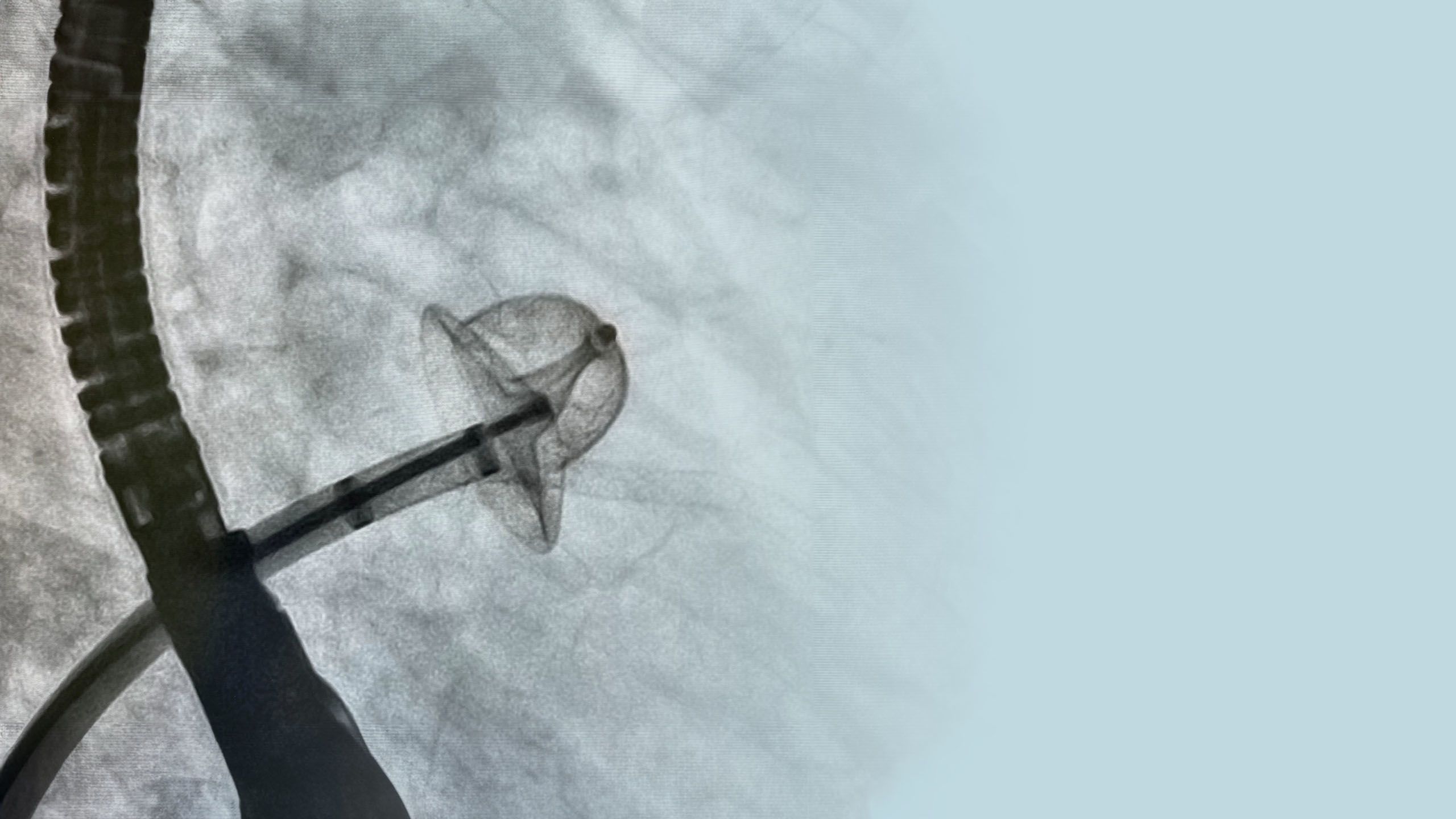
In addition to anticoagulation, LAA closure techniques have emerged as noteworthy alternatives. In particular, percutaneous LAA closure using devices implanted via a catheter has gained traction. The Watchman and Amulet devices are commonly used and have shown efficacy in reducing stroke risk similarly to anticoagulants, with the added benefit of lowering major bleeding risks.
Clinical trials, such as PROTECT-AF and PREVAIL, have demonstrated the effectiveness of these devices, with long-term studies showing reduced complication rates due to advancements in technology and technique. For example, the Watchman device has been shown to decrease major bleeding by about 71% compared to warfarin.
While the procedure carries some risk, advances in device technology have minimised these risks. The second-generation Watchman Flex, evaluated in the Pinnacle Flex trial, reported a notably low complication rate of around 0.5%, highlighting significant improvements in safety.
Similarly, the Amulet device, tested head-to-head against the Watchman, showed comparable low complication rates. Most complications occurred with less experienced operators, but rates significantly improved after the first 10 cases, underscoring the importance of operator experience. Pericardial effusion remains rare with newer devices.
INDICATIONS FOR LAA OCCLUSION
Current indications for LAA occlusion include high stroke risk with contraindications or intolerance to long-term anticoagulation. This procedure is intended for patients with non-valvular AF who have a high CHA2DS2-VASc score and valid reasons for avoiding long-term anticoagulants, such as a high bleeding risk or difficulties managing anticoagulation.
The original Watchman device, featuring a nitinol frame with anchors and an open front, posed risks such as pericardial effusion due to sharp edges. The Watchman Flex addresses these issues with design improvements, including a closed front, additional anchors for stability, and a fabric cover to reduce thrombogenicity.
The Amulet device uses a lobe and disc mechanism with a double layer of protection, and its availability in various sizes broadens its applicability. Future advancements in LAA occlusion technology, such as the WaveCrest and Lambre devices, aim to enhance safety and efficacy further.
Images: Shutterstock.com

IMPLANTATION
Implantation of LAA closure devices involves several steps, starting with imaging via transoesophageal echocardiography (TEE) or CT scans to assess the LAA anatomy. During the procedure, a pigtail catheter visualises the appendage, followed by deployment of the Watchman device, which is preloaded in a sheath and deployed into the appendage. A tug test ensures secure anchoring, and post-deployment imaging checks for leaks.
Patients with a Watchman device typically require oral anticoagulation plus aspirin for 45 days, followed by dual antiplatelet therapy for up to six months, and then aspirin alone. Trials indicate that 96% of patients can discontinue full oral anticoagulation by 45 days. The Amulet device involves dual antiplatelet therapy without prior oral anticoagulation, transitioning to aspirin alone based on post-implant imaging results.
Surgical LAA closure, performed during open-heart surgery or via minimally invasive techniques, has also been used based on the assumption that removing the appendage reduces stroke risk. Recent studies support its effectiveness, particularly for patients undergoing cardiac surgery with a CHA2DS2-VASc score above 2.
ABCs RECOMMENDED
The Atrial Fibrillation Better Care (ABC) pathway, endorsed by international guidelines, emphasises a holistic approach to managing atrial fibrillation. Its three pillars are: 'A' for Anticoagulation/Avoiding stroke, 'B' for Better symptom control with patient-centred decisions on rate or rhythm control, and 'C' for managing Cardiovascular risk factors and Comorbidities, including lifestyle changes. This approach has been linked to improved clinical outcomes and reduced adverse events.
Building on this model, the European Society of Cardiology Council of Stroke recommends a post-stroke ABC pathway. This includes 'A' for Appropriate Antithrombotic therapy, 'B' for Better functional and psychological status, and 'C' for optimising Cardiovascular risk factors and Comorbidities, with a focus on lifestyle changes.
CONCLUSION
Advancements in LAA occlusion devices have significantly improved safety profiles for AFib patients at risk of stroke. Both the Watchman Flex and Amulet devices show low complication rates, with the choice between devices and techniques depending on patient-specific factors such as anatomy, stroke, and bleeding risks, as well as the operator's experience.

REFERENCES
Sulaiman, S, et al, 2023. Left Atrial Appendage Occlusion in the Elderly: Insights From PROTECT-AF, PREVAIL, and Continuous Access Registries. JACC: Clinical Electrophysiology, Vol. 9, No. 5, 2023. May 2023:669 – 676
Choi, SE, et al, 2023. Atrial fibrillation and stroke. Expert Review of Cardiovascular Therapy, 21:1, 35-56.
Ledwoch, J, et al, 2020. WATCHMAN versus ACP or Amulet devices for left atrial appendage occlusion: a sub-analysis of the multicentre LAARGE registry. EuroIntervention, Vol. 16, No. 11.
Piedmont Heart Institute, 2022. Atrial Fibrillation and Stroke (CME). YouTube video, May 12 2022: https://www.youtube.com/watch?v=6DVwUUuKjvE

