Original study
Endophthalmitis at Johannesburg academic hospitals: A descriptive study
M Ebrahim, MBChB (Stell.), FC Ophth(SA), Dip Ophth (SA), Dip PEC (SA), Registrar, Division of Ophthalmology, Department of Neurosciences, Faculty of Health Sciences, University of Witwatersrand, Johannesburg, South Africa.
ORCID: https://orcid.org/0009-0005-1021-244X
MMed dissertation by publication
A Makgotloe, MBBCh, FC Ophth, Academic Head, Division of Ophthalmology, The Sam and Dora Chair of Ophthalmology, University of the Witwatersrand, Clinical Head, Department of Ophthalmology & Vitreoretinal Service, Clinical Head, Department of Ophthalmology & Vitreoretinal Service, Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa.
ORCID: http://orcid.org/0000-0002-8193-3245
Corresponding author: Dr M Ebrahim, email Yaseen.ebrahim@hotmail.com
Introduction
Endophthalmitis remains the most dreaded complication of any intraocular procedure.1 Clinical symptoms include pain, redness and vision loss. The signs associated with endophthalmitis may vary according to severity. These signs are eyelid swelling, chemosis, conjunctival injection, relative afferent pupillary defect and vitritis. Toxins produced by the infecting bacteria and the host inflammatory response cause rapid and irreversible photoreceptor damage and ongoing effects can continue long after the ocular contents have been rendered sterile.2,3
Risk factors for the development of endophthalmitis after cataract surgery include: posterior capsular tear, prolonged procedure time, clear corneal sutureless incisions, temporal corneal incisions, wound leak, delaying post-operative antibiotics, topical anaesthesia, adnexal disease and diabetes mellitus.2 Other risk factors for the development of exogenous endophthalmitis include open globe injuries, post glaucoma surgery and post corneal transplantation.
The Endophthalmitis Vitrectomy Study (EVS) remains the only level one evidence on the subject.4 EVS reported that the most common presenting symptom was pain (74% of patients) and almost all patients had reported blurred vision. Afferent pupillary defects were present in 12%, corneal ring ulcer/infiltrate in 5%, and hypopyon in 86%.4,5,6,7
The clinical signs which are noted are varied depending on the time to presentation and the clinical setting within which the patient with endophthalmitis presents. Patients with a history of glaucoma tend to present later and there are no differences in culture positivity rates as well as final visual outcome in patients that present early or late for treatment.8
The prognosis of endophthalmitis is largely dependent on the causative organism.1 In the EVS, the most commonly isolated organism was coagulase negative staphylococcus epidermidis. This normal skin commensal has also been found in cultures in more recent series.9 In other clinical settings, a similar profile of organisms are usually isolated with the exception of patients who have had glaucoma drainage devices implanted.10
Over the years, patient care has evolved in terms of management protocols, technological improvements and pharmacological advances. Interventions such as prophylactic iodine, smaller ports for vitrectomy and intracameral cefuroxime and moxifloxacin have drastically improved the rates and outcomes of endophthalmitis.1,11,12,13 Rates of endophthalmitis vary across different countries and is dependent on the clinical setting. Post cataract surgery related endophthalmitis occurs in 0.04% of patients.1,14
The clinical training platform of the University of the Witwatersrand’s division of Ophthalmology includes three hospitals in Johannesburg, South Africa: Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), Chris Hani Baragwanath Academic Hospital (CHBAH) and Helen Joseph Hospital (HJH). These three hospitals are referral centres for cases requiring tertiary level care.
Endophthalmitis has never been studied in our setting before. We therefore decided to conduct a descriptive study of all cases of endophthalmitis which were managed in our three teaching hospitals.
Methods
A policy of notifying all cases of endophthalmitis has been implemented in all our three teaching hospitals. These notifications are reported to the University of the Witwatersrand Ophthalmology office and presented at our morbidity and mortality meetings.
A retrospective descriptive case series study was conducted of reported cases of endophthalmitis at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), Chris Hani Baragwanath Academic Hospital (CHBAH) and Helen Joseph Hospital (HJH) in Johannesburg, South Africa. Ethical clearance was approved by the Human Research Ethics Committee, University of the Witwatersrand (M211032). Ethics approval was also granted by all these three hospitals to collect data from patients’ records. The study was conducted in accordance with the declaration of Helsinki.
All patients who had an acute endophthalmitis and subsequently presented in our morbidity and mortality (M&M) meetings between January 2011 and December 2019 were included in the study. Eligible patients were identified from the minutes of these meetings. Clinical records of patients who met the inclusion criteria were retrieved from the three participating hospitals for analysis.
Descriptive statistics were used to present the data and statistical analysis was conducted using Statistical Package for Social Sciences (SPSS) version 28 and Microsoft Excel 2019.
Results
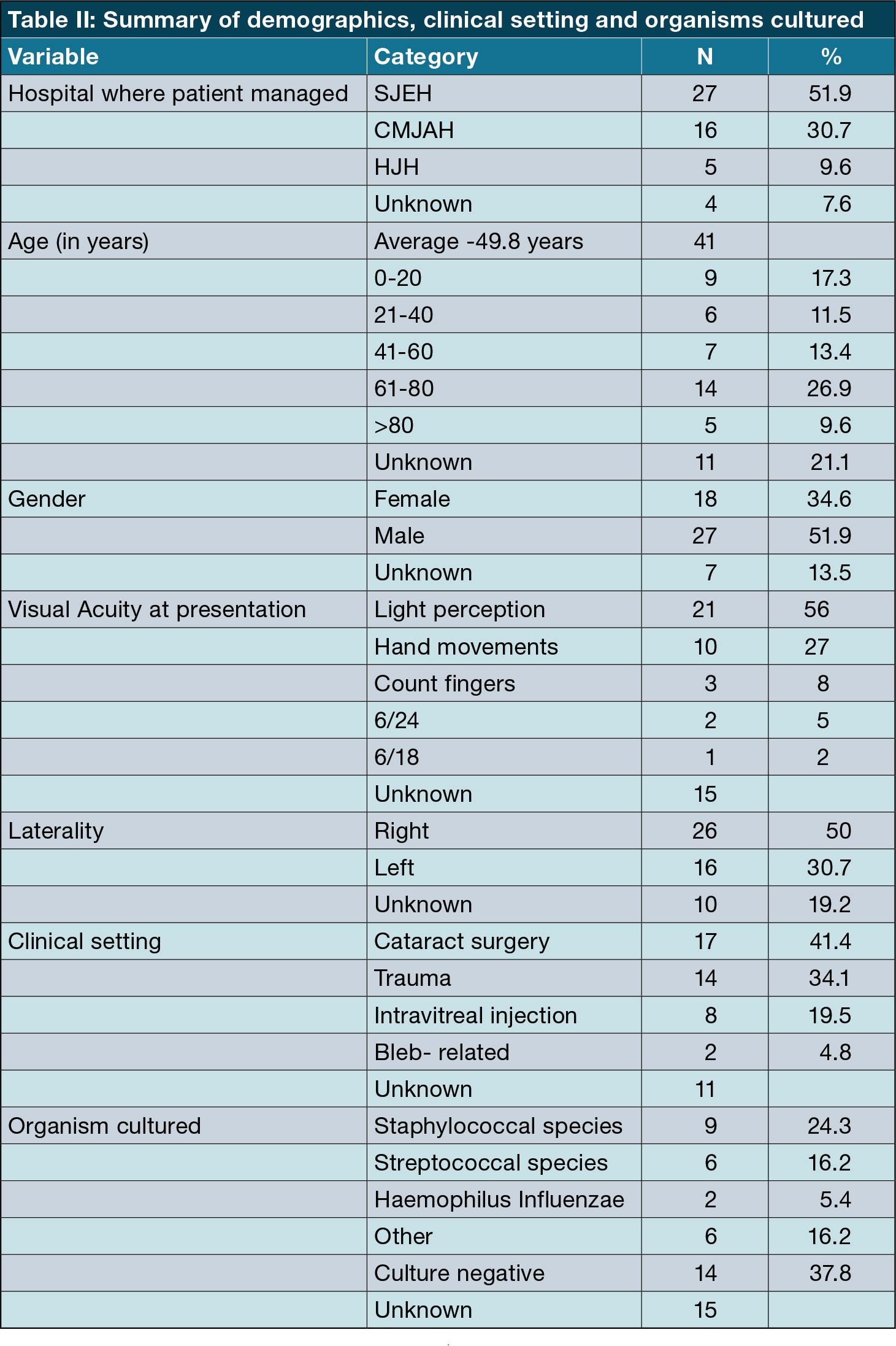
A total of 52 patients met the inclusion criteria for the study.
Gender
There were 18 females (34.6%), 27 males (51.9%) and the status of seven cases was unknown or not recorded (13.5%). A cross-tabulation analysis was done for gender. The results show that there does exist a relationship between gender and clinical setting (Fisher Exact Test significance of 0.001), ocular pain (<0.001), hypopyon (<0.001), AC Fibrin (0.027) and vitritis (<0.001).
Time to presentation
Fourteen records were missing data with regards to the number of days that elapsed between the development of symptoms and presentation to hospital and were therefore excluded from this analysis. Three patients had delayed onset post-operative endophthalmitis and were also excluded from the analysis. The mean time to presentation was 12 days (SD-16.0).
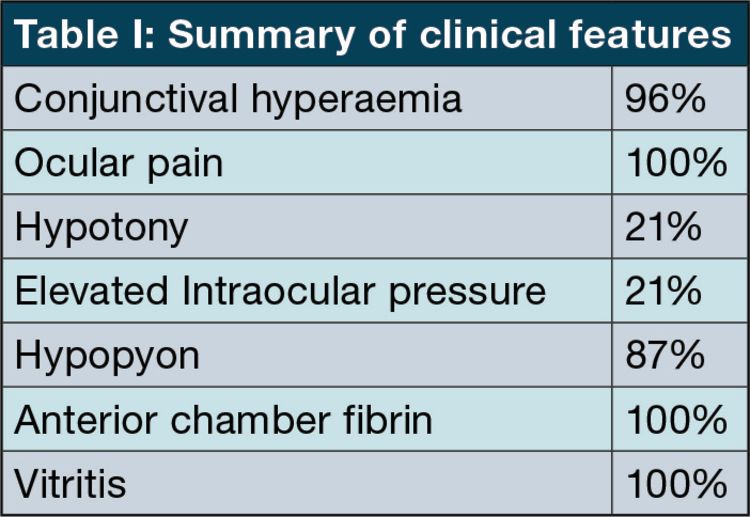
Presenting features
Organism cultured
Nine were Staphylococcal species: (Staphylococcus aureus- 4, staphylococcus epidermidis- 4, staphylococcus haemolytic- 1).
Six were Streptococcal species: (Streptococcus pneumoniae- 3, streptococcus viridans- 1, streptococcus mitis- 1, streptococcus anginosis- 1).
Two were Haemophilus Influenzae.
Six were “other” organisms.
Fourteen cultures did not yield a positive result.
Visual outcome
Due to poor follow-up of patients, absence of data of best spectacle-corrected visual acuity and continued visual rehabilitation after diagnosis, final visual acuity was not reported on in this study.
Four (7.6%) patients developed no-light perceptions due to phthisis bulbi or evisceration in this series.
See Table II for summary of findings for age, clinical setting and visual acuity at presentation.
Discussion
Despite the rare occurrence of endophthalmitis, and the limitations of retrospective analysis, it is important to constantly review the clinical features as well as the microbiological organisms associated with endophthalmitis in practice. This will assist in developing improved clinical protocols in the prevention and management of endophthalmitis.
The average age at presentation in this study was 49.84 (SD = 28.42). This study proved a statistically significant correlation between age and endophthalmitis in the clinical settings of both trauma and cataract surgery. This is consistent with numerous other studies showing extremes of age as being a risk factor for the development of endophthalmitis. This is postulated to be so in advanced age due to reduced natural immunity and younger patients requiring more complex surgery.1,14
This series, in line with other studies, found a male preponderance of endophthalmitis. Possible reasons for this include behavioural differences in adherence to post-operative instructions and compliance to treatment regimens.6
Fifty six percent of patients in this study had light-perception vision on presentation. This is in keeping with the delayed presentation and therefore the majority of patients will require a surgical intervention as part of their initial management. Delayed presentation also has a direct effect on final visual outcome.4,8
This series demonstrated a higher prevalence of endophthalmitis in patients undergoing extracapsular cataract surgery compared to phacoemulsification. A similar trend was reported by Lundström et al. who demonstrated that extracapsular or intracapsular cataract surgery had an approximately two times more risk of endophthalmitis when compared to phacoemulsification surgery.8
Endophthalmitis following intravitreal injections presents earlier than post cataract surgery which conformed to the findings of this study. All intravitreal injections are given in a ‘clean room’ in our department and monocular patients are given intravitreal injections in a theatre setting. No clear guideline exists for administering of intravitreal injections. A large review by Merani et al. advises that a sterile technique with the use of a povidone-iodine solution, omission of peri-procedural antibiotics, and wearing a mask or maintaining silence during the procedure to eliminate aerosolization of bacteria.15
Trauma places a major burden on the South African health care system with young males being most commonly affected. Alcohol is closely linked to incidents of non-accidental injury and the victims and assailants are commonly known to each other.16,17,18 This series confirmed findings of other South African-based studies showing an increased proportion of young males being affected by trauma resulting in open globe injury. The ocular trauma score as proposed by Kuhn et al. places endophthalmitis as the second most important sign as a poor prognostic indicator for vision after globe rupture.19,16 The EVS is only prescriptive with regards to post cataract surgery related endophthalmitis and no clear evidence-based guidelines exists for the management of endophthalmitis in other clinical settings.13
Our study showed a 62.2% culture positivity rate. In the EVS, a 69% culture positivity was achieved. More recent series show culture positivity to range between 33-56%. These lower rates were attributed to the fact that the EVS used vitrectomy as well as needle aspiration to collect samples, whereas current vitreous sampling methods only employ needle aspiration. Aqueous sample rates are significantly less culture-positive than vitreous samples.1,5
The EVS and the French Institutional Endophthalmitis Study (FRIENDS) found a similar rate of 94% Gram-positive bacteria in acute endophthalmitis after cataract surgery, and among them, 70% were coagulase- negative staphylococci belonging to the commensal flora.20,21,22 Our series also demonstrated a predominance of staphylococcal species identified from vitreous taps and 37% had culture-negative vitreous taps.
Mirzania et al. showed a worsening of the final visual acuity in patients who presented three or more days after onset of symptoms of endophthalmitis compared to patients who presented within two days of onset of symptoms. In our series, the average time to presentation was 12 days which lead to worse vision recordings at presentation and this ultimately led to the majority of patients requiring surgical intervention as opposed to more conservative measures.8
Pain is the most common symptom in this series and fibrin, hypopyon, conjunctival hyperaemia are the most common clinical signs.
The severity and outcome of postoperative endophthalmitis in cataract surgery mainly depend on several risk factors related to patients’ demographics such as old age, males, rural residence, and immunosuppressive conditions such as diabetes mellitus.5 The unfavourable visual outcomes of postoperative endophthalmitis in cataract surgery ranges from decreased visual acuity less than 6/60 to the loss of the eye.3 Final visual acuity was not reported on in this study due to poor follow-up of patients, absence of data of best spectacle-corrected visual acuity and continued visual rehabilitation after diagnosis.
Conclusion
Endophthalmitis is a rare and dreaded complication of any intraocular procedure that could lead to significant visual morbidity. The commonest type of exogenous endophthalmitis in our series was cataract surgery-related and the commonest organisms cultured were staphylococcal species. Unique to our study is the high proportion of trauma-related endophthalmitis and the late presentation of patients for ophthalmic care. Most patients had light perception at presentation requiring a surgical intervention. Four patients had developed phtisis bulbi or no light perception vision in this series.
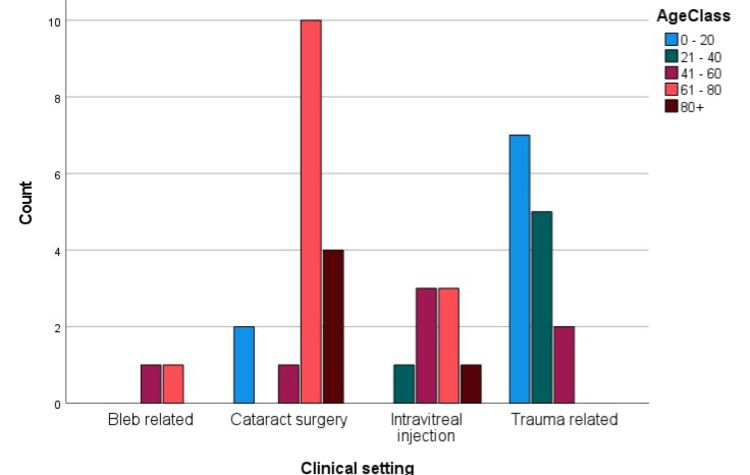
Figure 1: The relationship between age and clinical setting
Figure 1: The relationship between age and clinical setting
Limitations
The limitations of this study include its retrospective design, rarely occurring disease, small sample size, possible under-reporting of cases of endophthalmitis to the department and challenges with record-keeping in three different hospitals over a period of nine years.
Acknowledgements
Michael Paulse and Aasim Ebrahim for assistance with data analysis.
References
- Peck TJ, Patel SN, Ho AC. Endophthalmitis after cataract surgery: an update on recent advances. Curr Opin Ophthalmol. 2021;32(1):62-8.
- Bradley Bowling. Bradley Bowling – Kanski’s clinical ophthalmology – a systematic approach-Elsevier (2016). 2016.
- Zagaria MAE. Postoperative endophthalmitis after cataract surgery. US Pharm. 2016;41(4):8-11.
- Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study A Randomized Trial of Immediate Vitrectomy and of Intravenous Antibiotics for the Treatment of Postoperative Bacterial Endophthalmitis. Arch Ophthalmol. 1995;113:1479-1496. 1995;113(12):1479-96.
- Lundström M, Friling E, Montan P. Risk factors for endophthalmitis after cataract surgery: Predictors for causative organisms and visual outcomes. J Cataract Refract Surg. 2015 Nov 1;41(11):2410-6.
- Cao H, Zhang L, Li L, Lo SK. Risk Factors for Acute Endophthalmitis following Cataract Surgery: A Systematic Review and Meta-Analysis. PLoS One. 2013 Aug 26;8(8).
- Menikoff JA, Speaker MG, Marmor M, Raskin EM. A Case-control Study of Risk Factors for Postoperative Endophthalmitis. Ophthalmology. 1991;98(12):1761-8.
- Mirzania D, Fleming TL, Robbins CB, Feng HL, Fekrat S. Time to Presentation after Symptom Onset in Endophthalmitis: Clinical Features and Visual Outcomes. Ophthalmol Retin. 2021 Apr 1;5(4):324-9.
- Yannuzzi NA, Patel NA, Relhan N, Tran KD, Si N, Albini TA, et al. Clinical Features, Antibiotic Susceptibilities, and Treatment Outcomes of Endophthalmitis Caused by Staphylococcus epidermidis. Ophthalmol Retin [Internet]. 2018;2(5):396-400. Available from: https://doi.org/10.1016/j.oret.2017.08.025
- Rayess N, Obeid A, Storey PP, Juliano J, Rahimy E, Moshfeghi AA, et al. LONG-TERM VISUAL OUTCOMES AND CLINICAL FEATURES AFTER ANTI-VASCULAR ENDOTHELIAL GROWTH FACTOR INJECTION-RELATED ENDOPHTHALMITIS. Retina [Internet]. 2019 Nov 1 [cited 2021 May 22];39(11):2070-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30157114
- Ferguson AW, Scott JA, McGavigan J, Elton RA, McLean J, Schmidt U, et al. Comparison of 5% povidone-iodine solution against 1% povidone-iodine solution in preoperative cataract surgery antisepsis: A prospective randomised double blind study. Br J Ophthalmol. 2003;87(2):163-7.
- ESCRS Guidelines on prevention investigation and management of post operative endophthalmitis. B 2022 A et al. C 14(2): e22003. D 10. 7759/cureus. 2200. 6 of 8, P, Behrens-Baumann W, Pleyer U, Seal D (ed): The European Society for Cataract & Refractive Surgeons, Dublin I 2007. https://www. escrs. org/vienna2011/programme/handouts/i. 100/ic 100_barry_handout. pd. No Title.
- Relhan N, Forster RK, Flynn HW. Endophthalmitis: Then and Now. Am J Ophthalmol. 2018 Mar 1;187:xx-xxvii.
- Amoaku W, Bailey C, Downey L, Gale RP, Ghanchi F, Hamilton R, et al. Providing a safe and effective intravitreal treatment service: strategies for service delivery. Clin Ophthalmol. 2020;14:1315-28.
- Merani R, Hunyor AP. Endophthalmitis following intravitreal anti-vascular endothelial growth factor (VEGF) injection: A comprehensive review. Int J Retin Vitr. 2015;1(1):1-19.
- Gokce G, Sobaci G, Ozgonul C. Post-Traumatic Endophthalmitis: A Mini-Review. Semin Ophthalmol. 2015;30(5-6):470-4.
- Toit N Du, Mustak H, Levetan C. Open globe injuries in patients seen at Groote Schuur Hospital, Cape Town, South Africa. South African J Surg. 2013;51(3):97-101.
- Stuart K V., Dold C, van der Westhuizen DP, de Vasconcelos S. The epidemiology of ocular trauma in the Northern Cape, South Africa. African Vis Eye Heal. 2022;81(1):1-8.
- Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002 Jun;15(2):163-5 vi. doi: 10. 1016/s089. 1549(02)00007 x. P 12229231. No Title.
- Chiquet C, Bron AM, Lundström M, Maurin M. Acute postoperative endophthalmitis: Microbiology from the laboratory to the bedside. Surv Ophthalmol [Internet]. 2022;67(6):1698-710. Available from: https://doi.org/10.1016/j.survophthal.2022.07.001
- Hong BK, Lee CS, Van Gelder RN, Garg SJ. Emerging techniques for pathogen discovery in endophthalmitis. Curr Opin Ophthalmol. 2015;26(3):221-5.
- Shao EH, Yates WB, Ho I Van, Chang AA, Simunovic MP. Endophthalmitis: Changes in Presentation, Management and the Role of Early Vitrectomy. Ophthalmol Ther [Internet]. 2021;10(4):877-90. Available from: https://doi.org/10.1007/s40123-021-00406-6.