Notes on stroke:
Risk, recovery, and treatment
Stroke, the second leading cause of death and third leading cause of disability worldwide, poses an escalating burden, especially in low- and middle-income countries. Its prevalence and impact have surged over the past three decades, with a 70% rise in incidence, 85% in prevalence, and 43% in mortality, alongside a 32% increase in disability-adjusted life years (DALYs).
Low- and middle-income countries bear the brunt, experiencing a disproportionate 37% rise in stroke-related DALYs attributable to risk factors from 1990 to 2019. Concurrently, high-income countries witnessed a 25% decrease. This condition now ranks as the second leading cause of death and adult neurological disability globally, posing a significant healthcare challenge. Understanding the factors contributing to successful stroke outcomes and recovery is therefore paramount.
Low-income countries tend to exhibit a higher proportion of haemorrhagic strokes due to having a larger number of hypertensive disorders. However, as hypertension awareness and management improves, often accompanied by dietary changes, the incidence of haemorrhagic strokes decreases while the incidence of ischemic strokes and cardiovascular diseases increases.
RISK FACTORS FOR STROKE
In 2019, the primary risk factors for stroke included high systolic blood pressure, elevated body-mass index, increased fasting plasma glucose levels, exposure to ambient particulate matter, pollution, and smoking. Unlike myocardial infarction, which typically stems from large vessel atherosclerotic disease affecting coronary arteries, pinpointing stroke risk factors is complicated due to the various stroke types.
Essentially, stroke is categorised into haemorrhagic and ischaemic types, with approximately 80% being ischemic - though this ratio varies across populations. Haemorrhagic strokes may be intraparenchymal or subarachnoid, while ischemic strokes are further subdivided into aetiologic subtypes like cardioembolic, atherosclerotic, lacunar, and strokes of unknown cause.
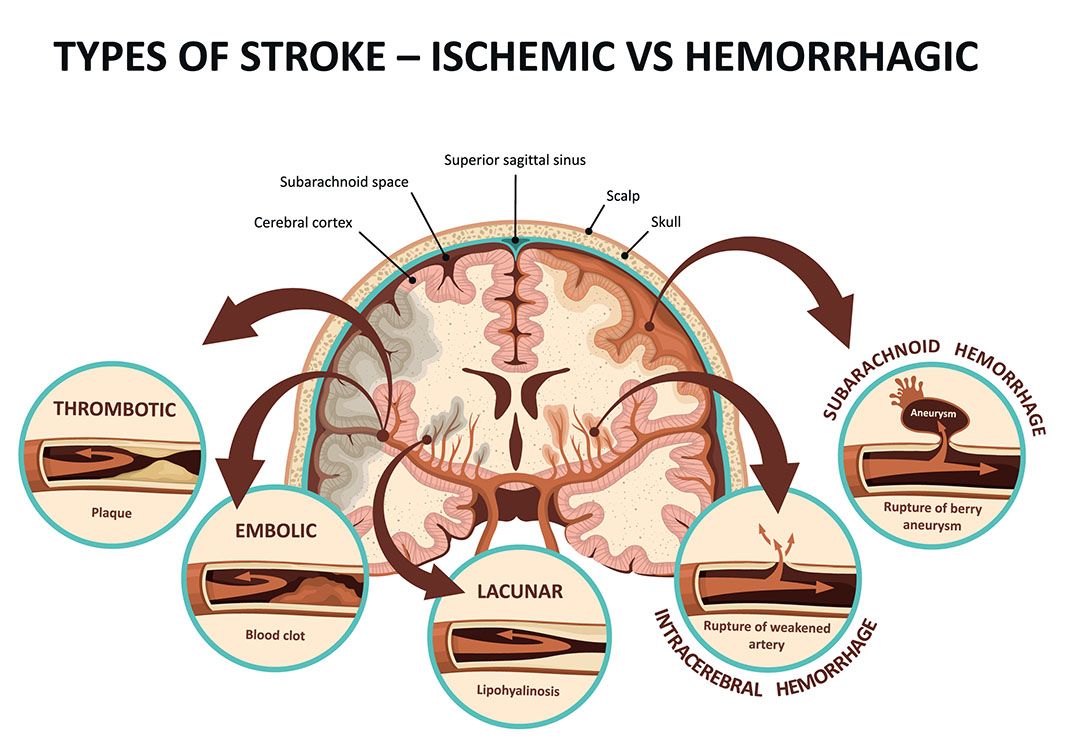
While risk factors for haemorrhagic and ischemic strokes share similarities, differences exist among ischemic stroke etiologic categories. Hypertension notably predisposes individuals to haemorrhagic stroke, although it also contributes to atherosclerotic disease leading to ischemic stroke. Conversely, hyperlipidaemia primarily raises the risk of stroke through atherosclerosis of both extracranial and intracranial blood vessels, akin to its impact on coronary arteries. Atrial fibrillation is also a key risk factor for cardioembolic stroke.
STROKE RECOVERY
Stroke recovery unfolds across distinct phases, each characterised by unique temporal dynamics. The initial 24 hours constitute the hyperacute phase, succeeded by the acute phase spanning the first week, followed by the early and late subacute phases extending up to six months post-stroke. Beyond six months lies the chronic phase, marked by stabilised deficits.
Early post-stroke, rapid neuroplastic changes promote recovery, particularly evident within the first few weeks. However, after three months, improvements in motor symptoms plateau, with subsequent progress slower and less substantial. Despite this, interventions can still yield gains even in the chronic phase, notably in cognitive domains like language.
However, categorising recovery into discrete phases oversimplifies a complex, non-linear process since variability exists both in the pace and extent of recovery among individuals. The widely accepted proportional recovery rule suggests that patients typically regain around 70% of lost function within three to six months post-stroke, irrespective of therapy intensity.
Yet, recent critique questions its validity, citing mathematical limitations and non-compliance among certain patients, especially those with severe deficits. Indeed, recovery trajectories differ widely among patients, influenced by factors such as perilesional oedema and diaschisis, which perturb functionally connected brain regions.
Advanced modelling approaches reveal that most stroke patients exhibit a combination of proportional-to-spared-function and constant recovery rather than strict adherence to the proportional recovery rule. Subgroup analyses further delineate distinct recovery profiles, hinting at underlying neurobiological mechanisms yet to be elucidated.
This complexity underscores the inadequacy of rigid phase-based models in capturing the intricacies of stroke recovery. Instead, a nuanced understanding acknowledging individual variability and continuous, multifaceted processes is imperative for optimizing stroke management and rehabilitation strategies.


TREATMENT STRATEGIES
Understanding the recovery process after a stroke is crucial for tailoring effective treatments, but it remains unclear why some patients recover better than others. A deeper understanding of the neurobiology behind different recovery patterns is essential for developing targeted treatment strategies to enhance functional outcomes post-stroke.

- Training-based interventions, including traditional therapies and innovative methods like mirror therapy or music-based therapy, have demonstrated varying degrees of success in promoting functional recovery after stroke.
- Manipulating brain activity has emerged as a promising approach. Techniques such as transcranial magnetic stimulation (TMS) or transcranial direct current stimulation (TDCS) can modulate neural plasticity, influencing activity across interconnected brain regions.
- Thrombolytic therapy, established as the standard for acute ischemic stroke following the NINDS tPA trial, demonstrated efficacy within a 3-hour window but carried risks of symptomatic haemorrhage. FDA approval in 1996 underscored its benefits despite risks. Subsequent research aimed to extend its use up to 4.5, 6, and 9 hours, including wake-up strokes. Concerns persist over haemorrhage risks and challenges in determining eligibility, especially with aphasia or fluctuating symptoms. Patients lacking a last known well time are often excluded. While some studies show positive outcomes, uncertainties remain regarding extended tPA use due to limited clinical benefits and eligibility complexities.
By targeting pathological network configurations observed after stroke, these interventions hold promise for improving outcomes. For example, inhibiting activity in the contralesional primary motor cortex (M1) using inhibitory repetitive TMS (rTMS) in stroke patients has been shown to reduce over-activity not only in the stimulated region but also in the ipsilesional hemisphere.
This normalisation of activity is associated with improved motor performance in the affected hand. Connectivity analyses further indicate that this normalisation is linked to a reduction in abnormal inhibitory influences from the contralesional M1, particularly in patients showing significant motor improvement.
PHARMACOLOGICAL THERAPIES
Regrettably, beyond conventional rehabilitation methods, there exists no widely endorsed pharmacological approach for stroke recovery. Lee et al conducted a meticulous systematic search and review to pinpoint the most reliable evidence regarding various registered pharmacological interventions aimed at enhancing post-stroke recovery.
Among the array of pharmacological interventions examined, only nimodipine for subarachnoid haemorrhage (SAH) exhibited compelling level A evidence indicating treatment efficacy, as per a comprehensive systematic review and network meta-analysis. However, other treatments supported by level A studies failed to demonstrate intervention superiority over control, including SSRIs, calcium antagonists, and citicoline for ischemic stroke, as well as magnesium, colony-stimulating factors, and GABA agonists for ischemic or haemorrhagic stroke.
MLC601/MLC901
Four studies were included in Lee et al examining the biologic treatment MLC601/MLC901. In an RCT involving 150 patients with ischemic stroke within 1 month of onset, participants were assigned to either MLC601 or placebo for 3 months. Results from repeated measures analysis revealed significantly higher motor recovery on FMA in treated patients at 4, 8, and 12 weeks compared to controls (LOE B-R).
A systematic review and meta-analysis of five RCTs comprising 1936 individuals favored MLC601 for functional recovery at the end of treatment, with a relative risk of 1.64 (95% CI 1.05–2.57; p = 0.031; LOE B-R). The confidence interval was prioritized for result interpretation over the prediction interval.
A long-term follow-up study of 880 ischemic stroke patients demonstrated increased odds ratios of functional independence at 6 and 18 months post-treatment with MLC601 compared to placebo (LOE B-R). In patients with ICH, a cohort study (n = 66) indicated sustained neurological and functional recovery effects with MLC601/MLC901.
PROMISING TREATMENTS FOR LACUNAR STROKE
LACI-2, a preliminary study involving over 350 patients who had suffered lacunar strokes, characterised by small blood vessel occlusion in the brain, evaluated the safety and efficacy of two commonly prescribed cardiovascular medications: cilostazol and isosorbide mononitrate. Administered individually or in combination, these medications were found to be well tolerated and safe, potentially offering improvements in patient outcomes.
Participants, averaging 64 years of age with a 31% female representation, were recruited from 26 stroke centres across the United Kingdom. They continued their usual prescribed medications, including those targeting blood clotting, blood pressure, and cholesterol, in line with stroke management guidelines.
Patients were randomly assigned to one of four groups receiving either isosorbide mononitrate alone, cilostazol alone, both medications, or neither, for a year. Regular phone surveys assessed health status, cognitive function, symptoms, and quality of life, supplemented by brain imaging at 12 months.
The study, deemed feasible for larger trials, demonstrated high adherence to medication protocols, with 95% compliance observed. Safety parameters were met, with few adverse events, including four deaths, minimal bleeding episodes, and no significant falls or dizziness. Expected mild symptoms like headaches occurred.
Potential benefits emerged, notably in the combined medication group, showing reduced dependency in daily living tasks, decreased cognitive impairment, and improved mood and quality of life. Isosorbide mononitrate alone reduced recurrent strokes and cognitive impairment, while cilostazol alone lessened the need for daily assistance.
These findings highlight the promise of these medications in mitigating the consequences of lacunar strokes, warranting further investigation to confirm their efficacy and elucidate their mechanisms of action in larger-scale trials.
Images: Shutterstock.com

REFERENCES
Boehme, AK, et al, 2017. Stroke Risk Factors, Genetics, and Prevention. Circ Res. 2017 Feb 3; 120(3): 472–495.
Endovascular Today, 2023. “Cilostazol and Isosorbide Mononitrate Evaluated as Therapy for Lacunar Stroke in LACI-2 Preliminary Study.” Bryn Mawr Communications, 9 Feb. 2023, accessed at: evtoday.com/news/cilostazol-and-isosorbide-mononitrate-evaluated-as-therapy-for-lacunar-stroke-in-laci-2-preliminary-study.
Lee, TH, et al, 2024. A systematic-search-and-review of registered pharmacological therapies investigated to improve neuro-recovery after a stroke. Front. Neurol. 15:1346177.
Grefkes, C, et al, 2020. Recovery from stroke: current concepts and future perspectives. Neurological Research and Practice (2020) 2:17.
Hollist, M, et al, 2021. Acute Stroke Management: Overview and Recent Updates. Aging Dis. 2021 Jul 1;12(4):1000-1009.
Rosenich, E, et al, 2020. Cognitive Reserve as an Emerging Concept in Stroke Recovery. Neurorehabilitation and Neural Repair. 2020;34(3):187-199.