Managing asthma
As new research emerges and guidelines get updated, our approach to asthma is in a state of constant change.

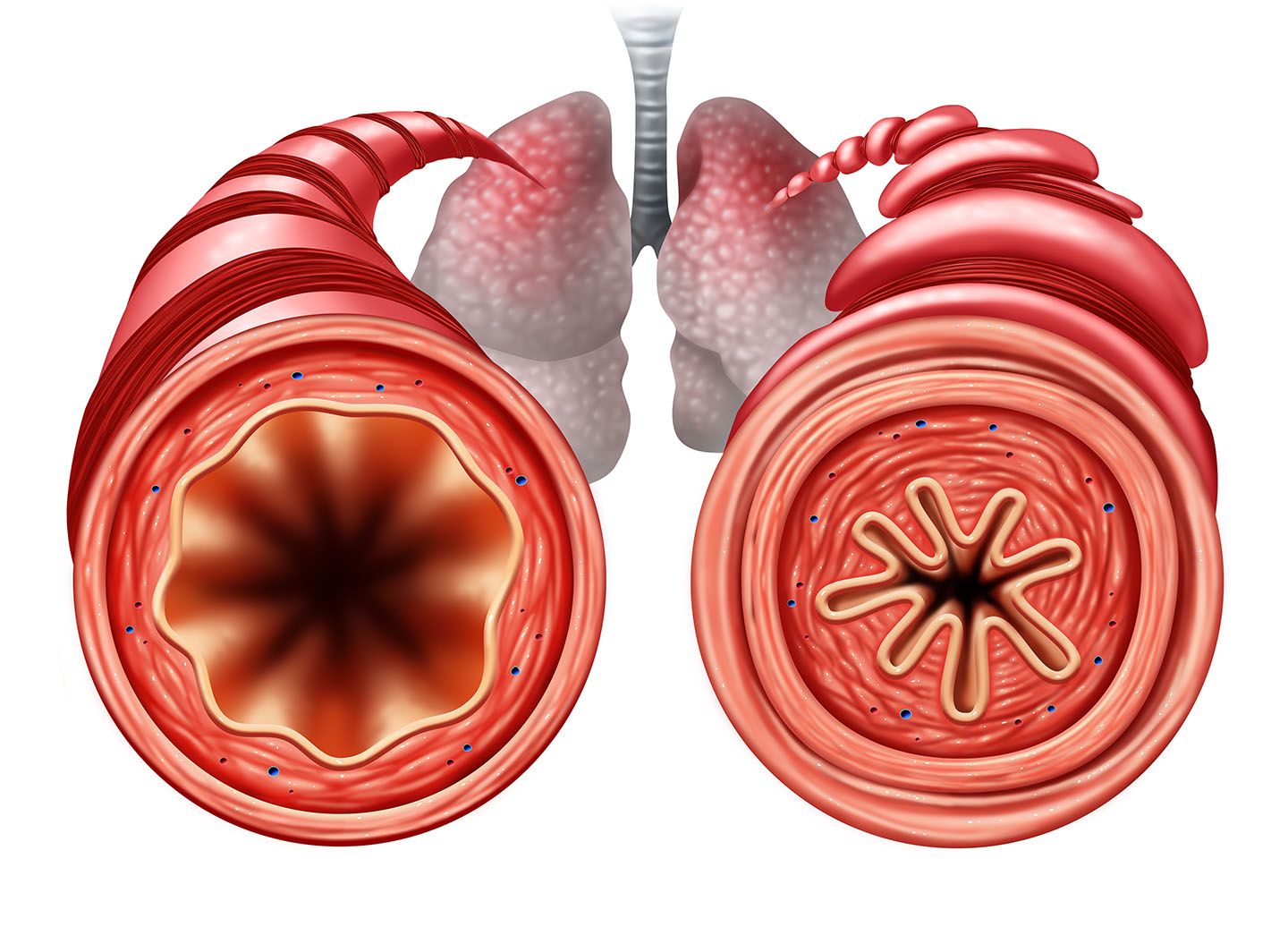
Asthma is a chronic condition characterised by persistent inflammation of the airways, which results in symptoms such as wheezing, breathlessness, chest tightness, and coughing. These symptoms can fluctuate in severity and frequency, requiring ongoing and tailored treatment to reduce symptom burden, prevent adverse events like exacerbations, and mitigate treatment side effects.
Asthma management follows a stepwise approach that centres around controlling symptoms and preventing exacerbations. This approach involves an iterative cycle of assessing symptoms and risk factors, adjusting treatments (both pharmacological and non-pharmacological), and reviewing responses to treatment. A successful asthma management plan is a partnership between the healthcare provider and the patient, incorporating patient preferences and individual treatment goals.

Pharmacological approach
Asthma treatments are divided into two main categories: control medications and relievers. Control medications, such as inhaled corticosteroids (ICS), are the cornerstone of asthma management. They work by reducing airway inflammation and preventing symptoms. Relievers, on the other hand, such as short-acting beta-agonists (SABAs), provide rapid relief from acute symptoms by relaxing the airway muscles.
Historically, SABAs were recommended as first-line treatment for mild asthma, primarily to provide quick symptom relief rather than address the underlying inflammation. This approach, advocated by the Global Initiative for Asthma (GINA) since its guidelines were first published in 1995, focused on managing bronchoconstriction rather than the inflammatory component of asthma.
However, in 2019, GINA revised its guidelines to address the limitations of this strategy. The updated guidelines introduced the concept of an anti-inflammatory reliever, which is crucial for managing asthma across all levels of severity. This approach enhances treatment efficacy and reduces the risk associated with over-reliance on SABAs.
Controller and reliever therapies
Before 2017, the GINA guidelines prescribed a controller medication (ICS) with a SABA as an additional rescue treatment. The SABA was seen as a supplementary option when the primary controller failed. While SABAs are effective for immediate symptom relief, they do not address the underlying inflammation, which requires consistent use of ICS.
“The updated guidelines introduced the concept of an anti-inflammatory reliever, which is crucial for managing asthma across all levels of severity.”
The introduction of the combination of ICS with long-acting beta-agonists (LABAs) marked a significant advancement in asthma therapy. This combination therapy, particularly the use of formoterol (a rapid-acting LABA) with ICS, has been shown to improve asthma control and reduce both severe and mild exacerbation rates. The FACET study demonstrated that adding formoterol to ICS reduced exacerbation rates significantly, irrespective of the ICS dose.


Adherence and real-world challenges
Adherence to asthma therapy remains a challenge, particularly with a strategy that requires regular use of controller medication. Surveys reveal a common pattern where patients use inhaled medications only when symptoms arise, leading to overuse of reliever medications and inadequate control of inflammation. Over-reliance on SABAs has been associated with an increased risk of severe asthma outcomes, including death.

In patients with mild persistent asthma, the addition of low-dose ICS can significantly reduce the risk of severe exacerbations and improve symptom control. If low-dose ICS are insufficient, combining them with LABAs (such as formoterol) becomes the preferred treatment. The SMART (Single Maintenance and Reliever Therapy) approach, which involves using a combination of low-dose ICS and formoterol as both maintenance and reliever therapy, is effective across all severity levels of asthma.
Inflammation
Asthma is not only characterised by bronchoconstriction but also by underlying inflammation. For instance, viral infections, such as those caused by rhinoviruses, can interfere with corticosteroid action, making anti-inflammatory treatment temporarily ineffective. This can lead to uncontrolled inflammation and exacerbations despite optimal use of controller medications. In such cases, temporarily increasing the ICS dose may help overcome transient steroid insensitivity and manage inflammation more effectively.
Research indicates that inflammation is a key factor in asthma symptoms and exacerbations. Elevated eosinophil levels and other inflammatory markers are associated with symptomatic asthma. Therefore, a transient increase in ICS dosage during periods of deteriorated control can prevent exacerbations and maintain better asthma control.
Paediatric considerations
Managing asthma in children, especially those under five, requires careful consideration of treatment options. The GINA guidelines suggest using low-dose ICS as first-line therapy, with leukotriene receptor antagonists added if control is not achieved. LABAs are not recommended for children under five due to safety concerns and the lack of approved alternatives. Off-label use of ICS is common in this age group due to the absence of suitable alternatives.
Studies highlight the importance of ensuring that medications effectively reach their target: the airways. Proper inhaler technique and adherence are critical, as poor technique can lead to inadequate medication delivery and poor asthma control. Regular follow-ups are essential to assess asthma control and adjust treatment as needed. Monitoring tools such as the Asthma Control Test and peak flow meters play a vital role in evaluating treatment efficacy.
Extra-fine particle ICS formulations
Recent studies have shown that extra-fine particle ICS formulations can provide better control and fewer exacerbations compared to standard-sized particles. This is particularly relevant for patients with smaller airways.
In practical terms, if a patient's current regimen, such as beclometasone, is effectively managing their asthma without excessive doses, it is advisable to continue with it. Addressing specific triggers, such as dust allergies, through measures like immunotherapy can further enhance asthma control. If patients relocate to higher altitudes, their asthma management plan may require adjustment due to changes in environmental conditions.
Conclusion
Effective asthma management involves a comprehensive approach that includes accurate diagnosis, personalised treatment plans, and continuous patient-provider communication. By understanding and addressing the various factors influencing asthma, from environmental triggers to individual responses to medications, healthcare providers can improve outcomes and quality of life for asthma patients. Personalised treatment, regular follow-ups, and appropriate inhaler techniques are essential for maintaining control and ensuring optimal asthma management.
Images: Shutterstock.com


REFERENCES
Papi, A, et al, 2020. Treatment strategies for asthma: reshaping the concept of asthma management. Allergy Asthma Clin Immunol (2020) 16:75.
Reddel, HK, et al, 2021. A Practical Guide to Implementing SMART in Asthma Management. J Allergy Clin Immunol Pract, Vol 10, No 1S.

